by Gertrud U. Rey
On February 27, 2021, the FDA issued an emergency use authorization for a third SARS-CoV-2 vaccine. The vaccine was developed by Janssen Pharmaceutica, a Belgium-based division of Johnson & Johnson, in collaboration with Beth Israel Deaconess Medical Center in Boston. Perhaps the most exciting feature of this new vaccine is that it only requires one dose to be effective in inducing an immune response.
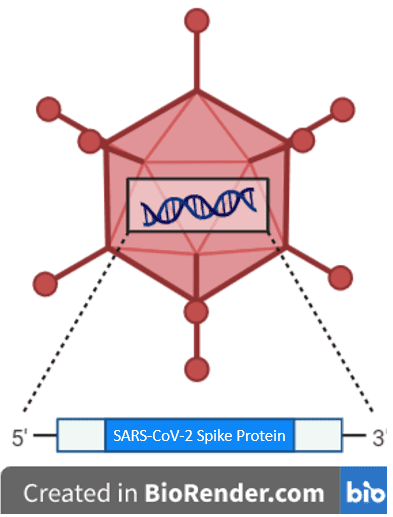
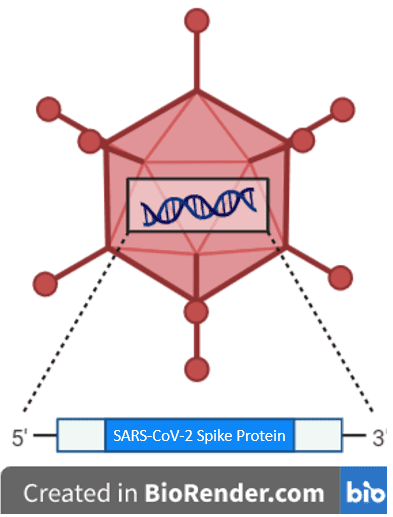
The vaccine is named Ad26.COV2.S because it consists of a human adenovirus vector, with a DNA genome, into which has been inserted the gene that encodes the full-length SARS-CoV-2 spike protein (pictured). Ad26.COV2.S is similar to AstraZeneca’s vaccine, based on a different adenovirus, and with a slightly different version of spike, which is not yet authorized in the U.S. The notion of using a virus as a vector to deliver vaccines to humans is based on the ability of viruses to enter cells by attaching to host cell receptors and releasing their genome into the cell. Upon injection into a vaccine recipient, the vaccine vector should enter cells and serve as a code for host proteins to synthesize the SARS-CoV-2 spike protein from the inserted gene. Ideally, the spike protein will then act as an antigen to prime the immune system to recognize SARS-CoV-2 if it infects the body at a later time.
Adenoviruses are particularly suitable as vectors for delivering foreign genes into cells because they have a double-stranded DNA genome that can accommodate relatively large segments of foreign DNA, and because they infect most cell types without integrating into the host genome. However, because of the prevalence of adenovirus infections in humans, most people have adenovirus-specific antibodies that could bind and neutralize these vectors, thus rendering them less effective at stimulating antibodies to the inserted gene product. AstraZeneca circumvented this issue by using an adenovirus of chimpanzee origin that does not normally infect humans. The adenovirus used to make Ad26.COV2.S (Adenovirus 26) is of human origin; however, when tested, most people have very few antibodies that inactivate this adenovirus, compared to antibodies against other adenoviruses. Thus, potential Ad26.COV2.S recipients are less likely to have pre-existing antibodies to the adenovirus vector itself. To optimize Adenovirus 26 for use as a vaccine vector, Janssen investigators deleted the gene that regulates viral replication, thus ensuring that the virus vector cannot cause an infection in human cells.
During infection, the SARS-CoV-2 viral particle fuses with the host cell membrane; a process that is mediated by two main events: 1) a structural rearrangement of the spike protein from its pre-fusion conformation; and, 2) cleavage of the spike protein by a cellular enzyme called furin. Based on the knowledge that the pre-fusion, uncleaved form of spike is more stable and immunogenic, Janssen investigators also inserted two mutations into the spike gene: one that locks the translated spike protein into its pre-fusion conformation, and one that prevents its cleavage by furin.
The FDA’s decision to issue an emergency use authorization for Ad26.COV2.S was based on safety and efficacy data from an ongoing Phase III clinical trial done in 39,321 participants who received either a single dose of Ad26.COV2.S or a placebo control. The trial was randomized, meaning that participants were randomly assigned to the experimental group receiving the Ad26.COV2.S vaccine, or the control group, so that the only expected differences between the experimental and control groups were the outcome variables studied (safety and efficacy). Randomizing trial participants eliminates unwanted effects that have nothing to do with the variables being analyzed. The trial was also double-blinded, meaning that neither the investigators nor the subjects knew who was receiving a particular treatment. Double-blinding leads to more authentic conclusions because they reduce researcher bias.
The basic findings of the trial were as follows:
- side effects related to vaccination were mild to moderate; and
- the vaccine was
- 66% effective at preventing moderate to severe COVID-19 across all geographic areas and age groups (U.S., South Africa, and six countries in Latin America);
- 72% effective at preventing moderate to severe COVID-19 across all age groups in the U.S.;
- 85% effective at preventing severe disease; and
- 100% effective at preventing COVID-19-related hospitalization and death as of day 28 after vaccination.
The apparently reduced efficacy of Ad26.COV2.S compared to the Moderna and Pfizer vaccines has led to considerable public skepticism. However, this is an unfair comparison for several reasons. Ad26.COV2.S was tested at a time when more variants were in circulation, including in places where the Moderna/Pfizer vaccines are thought to be less effective against locally circulating variants. Some limited data also suggest that Ad26.COV2.S might protect from asymptomatic infection and may thus prevent transmission from vaccinated individuals to non-vaccinated individuals. Although there is some evidence to suggest that the Pfizer vaccine has a similar effect, no such data exist yet for the Moderna vaccine.
The most critical measure of a vaccine’s efficacy is how well it prevents severe disease, hospitalizations, and deaths, and in this regard, all three vaccines are comparable. Moreover, Ad26.COV2.S has at least two advantages over the Pfizer/Moderna vaccines: 1) it does not require a freezer and can be stored in a refrigerator for up to three months; and, 2) it can be administered in a single dose. This will increase vaccine uptake, because people won’t have to get two shots and/or remember to get the second shot. It also makes it easier to immunize people with limited access to healthcare, such as the homeless and people living in remote areas. When all these factors are considered together, it is clear that Ad26.COV2.S will be a crucial additional tool in the fight against this pandemic.

I have two question about the use of the adenovirus as the backbone. 1, will previous exposures to adenovirus affect the efficacy of the J&J vaccine? 2, will getting the vaccine now affect potential responses to a follow-one, possibly annual SARS-CoV-2, vaccine also constructed on the same Ad26 backbone? This has been a concern of previous adenovirus vaccines.
1. Theoretically it should, but studies have shown that the general population has fairly low levels of neutralizing antibodies against Ad26. Neutralizing antibodies don’t just bind antigen, but they also inactivate it.
2. We don’t know the answer to this one, but one could simply get one of the other vaccines as a booster. Also, there’s a good chance that we won’t need an annual SARS-CoV-2 vaccine because most likely this virus will become endemic and will just cause mild colds after second or third infections. Influenza is kind of in a class of its own as far as annual vaccines go because of its genome – it reassorts. This makes it unrecognizable to antibodies to other influenza viruses. This is unlikely to happen with SARS-CoV-2.
I would like to hear good definitions of moderate, severe disease and what kind of “disease” requires hospitalization, or results in death. Can you compare the 3 vaccine clinical results, with the different disease categories, even with the caveat of different variants in the populations?
Pingback: One and Done - Virology Hub
To what degree has research been able to show that the Ad26 DNA is never integrated into host DNA?
I’d like to know if this vaccine can affect our dna like I’ve heard and how it can be affected by modifying our dna with this vaccine. Also how long does the vaccine work for?
Thank you for this blog. I received my j&j vaccination yesterday (04/01/21), and I just want to tell the world that it stopped my chronic sweating\clamminess 5minutes after the shot! I don’t have health care, but I assume that I have this problem of sweating due to or diabetes or perhaps some infection. I’ve also noticed significant reduction of gastrointestinal pain and that horrible gnawing feeling in my stomach that keeps me up at night. It’s been years since I had a break from misery, this vaccine is helping me