In the introduction to their paper, published in the Journal of Virology, the authors note other problems with many of the studies of XMRV in CFS patients:
- Too small control populations
- Patient and control samples collected at different times
- Investigators generally not blinded to sample identity
- PCR assays that rely on conservation of viral sequence mainly used
- Limits of detection, reproducibility, and precision of assays unknown
- Controls for each step that would identify analysis not done
- Insufficient numbers of negative controls included
- No study included positive samples from the original 2009 patient cohort of Lombardi et al.
To address these issues, the authors collected blood from 105 CFS patients and 200 healthy volunteers in the Salt Lake City area. One hundred of the patients fulfilled both the CDC-Fukuda and the Canadian consensus criteria for diagnosis of ME/CFS. The patients were selected from a clinic that specializes in the diagnosis and management of CFS and fibromyalgia.
New blood samples were also collected (by a third party) from 14 patients from the original study by Lombardi et al. The samples were blinded for subsequent study. Detection of viral nucleic acids was done using four different PCR assays. Anti-XMRV antibodies in patient sera were detected by ELISA. Finally, virus growth from clinical specimens was attempted in cell culture. The authors used the multiple experimental approaches reported by Lombardi and colleagues.
Let’s go through the results of each assay separately.
PCR for viral nucleic acids. Four different quantitative PCR assays were developed that detect different regions of the viral genome. The assay for pol sequences has been used by several groups and is the most specific PCR assay for XMRV. Three other PCR assays were also used that target the LTR, gag and env regions of XMRV DNA. These assays could detect at least 5 viral copies of XMRV DNA. The precision and reproducibility of the PCR assays, as well as their specificity for XMRV, were also demonstrated. DNA prepared from white blood cells of 100 CFS patients and 200 controls were negative for XMRV. For every 96 PCR reactions, 12 water controls were included; these were always negative for XMRV DNA.
XMRV antibodies in human sera. To detect XMRV antibodies in human serum, a portion of the viral envelope protein, called SU, was expressed in cells and purified from the cell culture medium. The SU protein was attached to plastic supports, and human serum was added. Any anti-XMRV antibodies in human sera will attach to the SU protein and can subsequently be detected by a colorimetric assay (we have discussed this type of assay previously). This assay revealed no differences in the amount of bound human antibodies for sera from CFS patients or healthy controls. Some of the patient sera were also used in western blot analysis. Recombinant XMRV SU protein was fractionated by gel electrophoresis. The protein on the gel is then transferred to a membrane which is mixed with human serum. If there are anti-XMRV antibodies in the human serum, they will react with the SU protein on the membrane, and can be detected by a colorimetric assay. When rabbit anti-XMRV serum was used in this assay, the SU protein was readily detected. None of the human sera analyzed by this method were found to contain antibodies that detect SU protein.
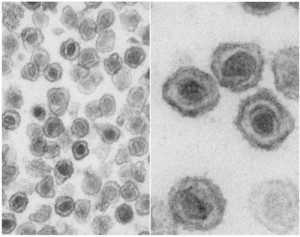
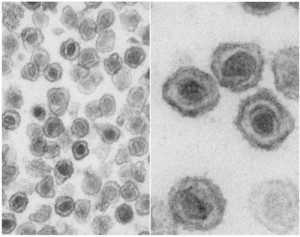
Infectious XMRV in human plasma. It has been suggested that the most sensitive method for detecting XMRV in patients is to inoculate cultured cells with clinical material and look for evidence of XMRV replication. The XMRV-susceptible cell line LNCaP was therefore infected with 0.1 ml of plasma from 31 patients and 34 healthy volunteers; negative and positive controls were also included. Viral replication was measured by western blot analysis and quantitative PCR. No viral protein or DNA was detected in any culture after incubation for up to 6 weeks.
Analysis of previously XMRV-positive samples. Blood was drawn from twenty-five patients who had tested positive for XMRV as reported by Lombardi et al. These samples were all found to be negative for XMRV DNA and antibodies by the PCR and ELISA assays described above. In addition, no infectious XMRV could be cultured from these 25 samples.
Presence of mouse DNA. After not finding XMRV using qPCR, serological, and viral culture assays, the authors used the nested PCR assay described by Lo et al. Although positives were observed, they were not consistent between different assays. This led the authors to look for contamination in their PCR reagents. After examination of each component, they found that two different versions of Taq polymerase, the enzyme used in PCR assays, contained trace amounts of mouse DNA.
Given the care with which these numerous assays were developed and conducted, it is possible to conclude with great certainty that the patient samples examined in this study do not contain XMRV DNA or antibodies to the virus. It’s not clear why the 14 patients resampled from the original Lombardi et al. study were negative for XMRV in this new study. The authors suggest one possibility: presence of “trace amounts of mouse DNA in the Taq polymerase enzymes used in these previous studies”. I believe that it is important to determine the source of XMRV in samples that have been previously tested positive for viral nucleic acid or antibodies. Without this information, questions about the involvement of XMRV in CFS will continue to linger in the minds of many non-scientists.
At the end of the manuscript the authors state their conclusion from this study:
Given the lack of evidence for XMRV or XMRV-like viruses in our cohort of CFS patients, as well as the lack of these viruses in a set of patients previously tested positive, we feel that that XMRV is not associated with CFS. We are forced to conclude that prescribing antiretroviral agents to CFS patients is insufficiently justified and potentially dangerous.
They also note that there is “still a wealth of prior data to encourage further research into the involvement of other infectious agents in CFS, and these efforts must continue.”
Clifford H. Shin, Lucinda Bateman, Robert Schlaberg, Ashley M. Bunker, Christopher J. Leonard, Ronald W. Hughen, Alan R. Light, Kathleen C. Light, & Ila R. Singh1* (2011). Absence of XMRV and other MLV-related viruses in patients with Chronic Fatigue Syndrome. Journal of Virology : 10.1128/JVI.00693-11

Thank you for answering my question by deliberately not answering the question. Why would I ever want or accept an explanation of how an assay was performed incorrectly by Singh et al from someone who has never run as assay like this in his/her life? At best you are parroting what someone else told you to say. Good luck to you, further discussion on this is pointless.
Am I getting this right?
– Prof. R. is basing his statement above on published information.
– You “correct” him and use a letter as proof of your assertion.
– When someone points out the mistake and shows you that the very same letter that you have provided as positive evidence of your assertion, tells the exact opposite of what you asserted, you reject that information becuse it is ‘just a letter and not published information.’
Please note that Van Kuppenveld states in the letter (that YOU thought was good enough to use as evidence) that he could detect it in “a cell line [<—22Rv1], as well as in positive samples [<— not 22Rv1] that were provided to us by Dr. Judy Mikovits".
Kay: If the original Science paper was flawed, it’s not really correct to say that Science made a “huge mistake” in publishing it in the first place. The journal is reponsible for due diligence in reviewing an article and arranging for appropriate peer review, not for using psychic powers to peer into the future and see if one paper’s conclusions will later be questioned or disproved by subsequent research.
I hate to use that fatuous phrase “That’s how science works,” but, well, that’s how science works. Even negative results add to the body of knowledge. Even results that later turn out to be mistaken or misleading add to the body of knowledge. (The reason I call the phrase ‘fatuous’ is because it’s been used as a weapon of condescension against patients who are anxious about political considerations or other factors hindering the course of research. Conspiracy theorists go way too far with this, of course, but it’s perfectly correct to say that politics HAS hindered the course of research on this disease in the past, and patients’ concerns that ME/CFS research might go back to being neglected entirely if the XMRV line of inquiry doesn’t pan out…well, they’re based on history. Nobody wants a repeat of the Stephen Straus
debacle.)
Please see comments below
Your comments are therefore built from your emotions not the data.
This is very funny coming from you, as I have seen that you and others on the forums have only just found out that this 67% result was “just” found using PCR techniques and did not involve culturing. So I’ll take your statement about what I do or don’t understand as a compliment.
And your logic is non-existent. When Singh had indeed stated that she had used the same RT-PCR assay instead of the same PCR assay, you could have said exactly the same thing as you do now (‘several papers have claimed to have used the same methodology, they did not’), which renders your argument invalid.
LJ: “the statements of a small vocal minority of a few thousand extreme CFS patients.”
It’s not a few thousand. It’s not even a few hundred. It’s really a few *dozen* that are this extreme and this bullheaded about their tribal loyalty that they’ll go into such a reactionary frenzy over a paper so carefully and meticulously done, published by a group of highly respected and credible researchers.
“The basic problem here is people with CFS have very few places to turn
for help for there real physical disease. There are only a handful of
specialist in the US for millions of patients. When people are left to
there own devices for a disease that has derailed their life some are
willing to accept any hypnosis or treatment that sounds plausible to
them out of desperation.”
Yes, yes, yes, a thousand times yes. Sometimes people wonder why I am so adamant about rejecting any form of “alternative” therapy for ME/CFS – my doctor was taken aback when she suggested she could get me referred for acupuncture (which my health plan covers) and I said NO, I DO NOT WANT ACUPUNCTURE. Not only do I think acupuncture is bunk; I am also perpetually offended by the fact that the “alternative” treatments are in fact not “alternative” at all for us; they are our *only* option, apart from the little bits of palliative care that mainstream medicine sometimes grudgingly offers us. People don’t walk into a (legitimate) doctor’s office with cancer or heart disease and get told, “Well, there are no FDA-approved treatments for your condition, but we can get you ACUPUNCTURE! Aren’t you excited?”
It’s not just patient desparation that drives this. We get pressure all the time from others that we should be “doing more” to try to help ourselves. Nobody wants to believe that there really isn’t that much out there; that we really are in a wilderness without access to meaningful medical care. Personally, I have opted to skip the step where I empty out my meager life savings and make myself sicker expending the energy to run from quack to quack and try every form of snake oil on the market before giving up and just opting to take the best care of myself that I can. And yet you wouldn’t believe the side-eye I get from some people: “How do you know it won’t help until you try it?” “There must be SOMETHING that will help.” “I think you’re being closed-minded.”
Dr Racaniello was wrong. They did not publish the data, but have admitted to it.
22Rv1 is not a clinically positive sample and has been treated with testosterone, which will have increased the viral titre to levels detectable with such an assay. This is your mistake.
It’s refreshing to see the rational voice in the CFS community. Kudos to you LJ.
Eric: “I’d rather have every patient donate to good research than paying a lot
for experimental treatments and becoming an expert of the disease, but
without knowing how to defeat it. ”
I’d rather have our public health agencies use our hard-earned taxpayer dollars to actually protect the public health instead of placing the onus on patients to fund research for their own debilitating, disabling disease. But I may have mentioned that once or twice before 😉
There is no mention of RT-PCR in Shin et al. Mark, have you read Mikovtis et al, that paper was published months ago and may be a little easier for you to understand.
Lombardi et al
“We isolated nucleic acids from PBMCs and assayed the samples for XMRV gag sequences by nested polymerase chain reaction (PCR) (5, 6). Of the 101 CFS samples analyzed, 68 (67%) contained XMRV gag sequences.”
5 is Urisman, 6 is the supporting material for Lombardi.
Lombardi supporting material
“Nested RT-PCR for gag sequences was done as described (5) with modifications. GAG-O-R primer was used for 1st strand synthesis; cycle conditions were 52oC annealing, for 35 cycles. For second round PCR,
annealing was at 54oC for 35 cycles.”
Urisman used Nested RT-PCR for gag.
Shin et al does not mention Nested RT-PCR anywhere.
” For the nested PCR, we made 2 modifications to the original protocol (11). We used 1.0 U of Platinum Taq instead of 0.5 U, and added dUTP to the mastermix to prevent subsequent PCR contamination with amplicons.”
1. I have done some basic research and I have found not one single correct scientific validation using your method. Of course, with your proper scientific insights, you will know that the onus of proof is on you, as I can never positively prove that there are no such findings (just as you cannot prove that there are no yellow swans with purple dots), but if I am wrong, it takes only one example from you to prove me wrong. So please provide us with that one, single example in the history of virology.
That you cannot provide me with such an example on multiple occasions and resort to the (unscientifc) ‘try passing it through the regulators’ soundbite is very telling.
For your information, a scientific finding doesn’t ‘pass through regulators’ when it is in the process of being validated. Only after a finding is validated, people will try to ‘pass it through regulators’.
2. When you reread my post, you’ll see that I am actually paraphrasing you. When people use quotes, it is a sign that it’s actually not their opinions that are being presented, but the opinions of others. My argument is that you implicitly accuse Mikovist of being a lousy scientist, using your quotes to support that assertion. I am at least glad to see that you do not dispute this assertion.
@8a90d80b158dc322ad78fb0d98bd979c:disqus : DOLPHIN THERAPY?? Sign me up! I want some of that dolphin therapy!
Seriously: I’ve always said that if all I can get for ME/CFS are placebos, I’d rather pick my own, ones I already know I like. Reading, writing, thinking, taking pictures (when I’m able, which is not often), spending time with friends (when I’m able, which is not often). All these things take way more effort than they would for a healthy person, but at least they won’t bankrupt me or tempt me to think I’ve found a “cure.” I feel temporarily better when I play with a friend’s kitten, so I think dolphin therapy sounds awesome.
In Lo et al, how many people who tested positive via RT-PCR also tested positive by DNA PCR and vice versa? Your argument that RT-PCR is somehow definitive would have to mean that it is common to detect viral RNA but not DNA.
How would serology be affected by “virus breaking up”? There was a pedigreed negative control that tested antibody positive and negative on samples taken two days apart, and a putatively positive person who also had different results on samples taken two days apart. These data indicate that the antibody test is not reliable, and furthermore also suggests that the issue is unlikely to just be cross-reactions given that the samples were taken just two days apart and it is extremely implausible that any antibody response would wax and wane in this time frame.
Glad to see you have googled and have visited Laika’s blog. My name is not Mark but I use an email address with that name in it to post there and elsewhere. You just never know. Thank you for proving my point.
No need for the condescending tone, as you are the one not correctly understanding things. Nothing you state above adresses, let alone invalidates the argument in my previous post, so please reread and reconsider your reply.
You don’t address the argument.
Van Kuppenveld stated that he could detect it in 22Rv1 AND in samples provided to him by Judy Mikovits.
I am sure an ad hoc hypothesis can be thought of that reduces any cognitive dissonance caused by your post.
The antibodies are at the limit if detection, or maybe something went wrong with collecting the sample without antibodies, or the way antibodies react to this virus is just different than everything we have ever seen. I’ll just stop here before they make me an honorary member at the mecfsforums.
Then you have not done the basic research required and your statement contradicts your earlier statements that there have been no replication studies. Validation cannot be claimed without proof, hence why you would never get such a study passed regulators. Shin et al did not meet the requirements that Singh herself suggested were appropriate back in November.
That you still cannot provide me with a single example is very telling.
Have you done the basic research? If so, why can’t you provide me with a single example?
You name is on this site.
You cannot argue with the published data, or you would be claiming that they Shin et al or Lombardi et al have some how lied.
I want to echo the statement of Drosha. 20 interwebz to you, LJ.
(And please note that there are also sane and kind people on the other side of the debate. I am also just a small but vocal minority. 😉 )
@kellylatta: I’m concerned with the careful use of language and rhetoric and how those affect the course of a discussion; you seem to be concerned with your “broader points” all being legitimate regardless of which particular words you chose.
I pointed out that you were using the word “antivirals” when you meant “antiretrovirals,” and that this detail actually does matter to the substance of the discussion, because the use of an antiviral or an antiretroviral is dependent on which theory of the disease you are pursuing, and at the present moment use of an antiretroviral would be based on a new, highly controversial, and unsubstantiated theory of the disease (XMRV), whereas use of antivirals is based on a theory of the disease (failure of the immune system to control chronic low-level infections) that has been around much longer – not uncontroversial itself; but there is a lot more data to suggest that something along the lines of these “subclinical” infections is present in ME/CFS.
I pointed out that “poisoning patients” was an over-dramatic rhetorical use of language; yes, I am aware that many drugs, including chemotherapy drugs, literally are “poisons.” (Another point of detail: Rituximab is not itself a “chemotherapy” drug: it’s a monoclonal antibody that’s used in conjunction with chemotherapy drugs in cancer patients – but you knew that too, right?) Of course, patients with cancer put up with this “poisoning” when there is nothing more benign available that will be effective. Fringe alternative-medicine types sometimes argue that their particular brand of anti-cancer snake oil is better than “conventional” treatments for cancer because chemotherapy is “poison”; while literally true, the wielding of this type of language in this instance is deliberately inflammatory and scaremongering.
None of this language and rhetoric is operating in a contextless vacuum. Many of those calling for extreme caution in trying any drug with significant side effects in CFS patients are delivering this message with a not-so-subtle subtext: this disease is not “serious” enough to warrant the use of such “serious” drugs; researchers and clinicians who want to try these drugs in patients are irresponsible and patients simply don’t understand the risks of side effects that would be worse than the mere “fatigue” they suffer. I feel sure that you do not have this intention, given the content of your other posts. But there is enough confusion and heated rhetoric around this topic already to warrant caution in your choice of words to make sure they are conveying the message that you intend.
Pingback: XMRV and YOU « TheScienceLink
This circular argument of yours does not make up for the absence of data in your beliefs.
That would support the findings of Lombardi et al, but was omitted from the published paper. They did not find contamination but the virus. 22Rv1 is not a clinically positive sample.
Ruscetti had this to say at the time, “I do not know how they
think they get away with this ethically,” said Ruscetti. “I do not think
this is good science.”
http://listserv.nodak.edu/cgi-bin/wa.exe?A2=ind1005a&L=co-cure&T=0&F=&S=&P=1724
Johan I feel sorry for you. You have no idea what you are talking about. Why not understand what ME is.
You use the term CFS to say all studies for XMRV have been on CFS. I am talking about ME G93.3 the neurological disease as listed by the WHO .
You do not understand the early days of AIDS and the politics as well as the difficulty of developing an accurate assay for a retrovirus. That is why you take my remarks completely out of context as if they are a personal attack on you.
If you are talking about “CFS” what definition i don’t know, instead of ME G93.3 this may be why you don’t understand how a retrovirus along with all the other medical abnormalities is the leading hypothesis.
Co infections etc being studied is great but will never be a substitute for developing a causation hypothesis and finding the actual cause.
Its obvious you cant see the difference and are happy to go along with the merry go round of a “mystery illness” that can implicate no one and be a cash cow for the status quo.
It is very telling that you say you haven’t seen any studies looking for a HGRV. Well if you ain’t looking for a HGRV you cant possibly find XMRV.
So is that why the 0/0 studies cant find xmrv because they are looking for a synthetic clone not a human retrovirus. Well that is the best explanation I have heard so far thank you for confirming it.
You are the epitome of the naive, everytime you open your mouth you show your ignorance. That’s why people who have as little understanding of science as you are easy to fool and therefore drag others along with you.
If you really believe that no XMRV studies have been done on people with ME that is laughable and your level of ignorance is a a gift that could only come down the chimney from Santa in a gigantic sized stocking.
Perhaps the 0/0 studies try to exclude as many people with ME as they can ie/ thew Wessely supplied one via Mclure and the Kuppfield one. However the whole purpose of these studies is to to find a new Human Gammretrovirus currently named XMRV in people with ME. The same family of retrovirus found by Lomabardi and Alter.
Because certain people are defining XMRV as a synthetic clone and looking for it in their samples is the very reason they cant find the lombardi HGRV named XMRV that Dr Mikovits consistently refers to as a HGRV.
Is that enough of and education for you?
Yes, Urbantravels, me too. But have they done so in the past? No. When will they do it? Do you want to wait until that moment and lose that time. Of course we should work towards getting them to give more, but what we have, we can give now and get work done now.
Dear RRM, Roy Hobbs, Kay, LJ, Drosha, etc,
Can one of you please show where these researchers demonstrated that their assays can detect XMRV in a clinical (not spiked) sample?
Yes, I know you are all very concerned about the “circular reasoning” of this question. But this is not a reason to avoid this question entirely (I’ve addressed this in another comment below). There is enough evidence to at least *suspect* that the WPI samples are positive. By not using the *exact same* methods as the WPI on these samples, the researchers introduced two questions/unknowns:
1) Do these samples actually contain XMRV?
2) Can the methods employed in this study detect XMRV in these samples if it is there?
As any 8th grade science student knows, science can only address one question/unknown at a time. Introducing more than one question/unknown at a time only creates confusion.
All of you (as well as the authors of this study) seem to be making the rather elementary mistake of concluding that this study answers question #1 by *assuming* that the answer to question #2 is “Yes.”
Furthermore, I find it thoroughly bizarre how painstakingly devoted your efforts are to shore up the narrative “consensus” that XMRV is over. Why?
Is it because you are worried about wasting valuable time and money on a “dead-end” theory?
Doubtful. If this were the reason you would also have to be up-in-arms about 90% of the research that goes on in academia with the primary purpose of keeping grant money flowing. Where were you when the UK spent $5M on the awful PACE trial? Where were you when Reeves and Wessely wasted untold monies on absurd psychosomatic studies? Nowhere, of course.
Is it because you are genuinely concerned about ME/CFS patients and the harm that ARV’s might cause?
Again, doubtful. Where is your concern over the abundance of unnecessary medications (some of equally potent composition) that are ingested in the Western world? What have you done or campaigned for that will help these patients you so apparently care for? Nothing, of course. All you do is deny, deny, deny and while offering conciliatory reassurances about “well, even though it’s not XMRV, more research should be done.” Of course, once you’re convinced that XMRV has been kicked to the curb, I’m sure we won’t see your faces around to follow through.
Is it because you have some deep-seated yearning for the “truth” and cannot stomach the idea of people pursuing theories you deem false?
Again, doubtful. If you did, you would also devote at least some effort to correcting any of the innumerable other questionable theories out in the world. But you don’t and instead are perversely fixated on this one small corner of the biomedical world. If it really is true (as many of you would have others believe) that the WPI is conducting “fringe” science and deluding a small handful of “crazy” patients, why does this matter? It certainly wouldn’t be close to the only contemporaneous example.
So please, spare us the faux concern and skeptical posturing.
A simple quesiton and i’ll ask it again. Maybe some of the authors of the most recent posts can answer it:
In the study discussed here, Dr. Singh has tested 200 healthy controls and 105 cases of ME/CFS. Result: 0 XMRV.
This contradicts her previous work in prostate cancer (4% XMRV positives in healthy controls, Schlaberg et al.) and probably also Bill Switzer’s most recent study (unless XMRV only appers in prostate cancer patients and never or almost never in healthy people, which would be a big warning sign on it’s own, wouldn’t it) here: http://www.plosone.org/article/info:doi/10.1371/journal.pone.0019065.
So, before it’s shown that Schlaberg et al. and Switzer et al. were wrong, how can you conclude Dr. Singh’s latest XMRV study is correct and call the case closed?
I don’t see it.
It’s not even necessary to test their assays against a WPI sample.
Both Dr. Singh and Bill Switzer have published studies where they reported finding XMRV.
Now they should use their assays from their negative studies and test the subjects they earlier found positive.
Roy without god coming down from heaven and giving you the answer you have to use as the most objective marker, the one can provide positive proof consistently. Then you can go from there. That is exactly how the Lipkin study is going to work. If you consistently come up with a positive on the same samples over and over again that is about as objective as you can get.
Those 14 positive samples by any mathematical probability would not be consistently positive if it was contamination. The WPI don’t only supply positives samples. They produce just as many negative ones. In all positive studies the ME patients and the healthy controls are handled in exactly the same way and they test positive at the rate of 70-80% in patients and 3-7% in healthy controls. That in itself is strong proof against contamination. I would say pretty much concrete proof. Wpi have also identified a cytokine profile in the ME patients that matches those who test positive for xmrv. None of this hits the mainstream media or certain journals or conferences because it doesn’t fit in with the contamination theories which are just that – theories.
Also you are not addressing the issue of Singhs assay being incapable of finding even population levels of XMRV in 300 samples which the CDC admit is an infectious virus and Switzer himself confirmed finding it in his 1.9% findings in prostate cancer.
This is an issue which people leaning towards contamination here just will not address.
Singh has found XMRV in prostate cancer so should be aware of the population level issue. She used a novel blood assay for this study one which has never proven to find XMRV previously. That does not provide objective proof of contamination in someone else’s study.
The only objective claim that can be made is that Singhs assay in this study was incapable of detection. Anything else claimed is purely a claim not an objective scientific conclusion.
If one does not agree with this one doesn’t agree with the scientific method.
Your post is contradicting itself. Replication, by definition, completely rules out calibrating your samples against known positives from the study you are trying to validate. You can promote independent replication, or you can promote calibrating to know positives, but you really cannot promote both at the same time.
Note that the WPI concluded that these samples contained XMRV without being able to calibrate their samples against their own results. It must then be possible for others to replicate this finding, at least if true, using the methodology that Lombardi et al. describe. Note that by calibrating to WPI’s “known positives’, you are not at all replicating WPI’s methodology as, again, calibrating to known positives part wasn’t part of the original methodology.
Since I will admit that your simgle post is more eloquent and well written than most of the other comments here, I will again ask, in the hope that you will prove me wrong:
If your proposed methodology is sound science, why can not one person give me a single historical example where a validation study did calibrate its assays to the supposed positives of the study it was trying to validate? If your argument is sound, then surely you can direct me to a single historical example of your proposed scientific methodology?
I think to know that you won’t find an example because it is circular thinking and thus bad science. Again, this supposed “problem” is not a problem at all because the original scientists behind any finding also came to their conclusions without having to rely on their (supposed) findings either. Thus, their findings can be replicated indepedently.
As for your thoughts about my personal motivations concerning all those things you mention, sorry to sound rude but I frankly couldn’t care less.
What does “passed regulators” mean? Who are the regulators you are talking about? The FDA? Why do you keep bringing this up?
– The samples from Phase IIa, where WPI (and CDC) found positives, were also freshly drawn
– All (or at least most) of the VipDx samples are also freshly drawn.
– The Alter/Lo retest samples were also freshly drawn. WPI also found XMRV in these samples.
Honest question: If you find that WPI tested their samples on Mondays and Singh tested her samples on Fridays (and everyting else was done the same), would that invalidate an “exact replication attempt” by Singh?
If not, why not?
The negative could now be positive. This will also be influenced by who the negative was.
It has been suggested that as infected cells are dying. They release bits into the plasma. Making it easier to detect as time passes.
“Yo
u can promote independent replication, or you can promote calibrating to know positives, but you really cannot promote both at the same time.”
Why has no one done this then?
“Note that the WPI concluded that these samples contained XMRV without being able to calibrate their samples against their own results. ”
You point is not clear at all.
The original methodology applied what was learnt from Urisman et al, but adapted to blood. Hence the reason for lowering the stringency of the primers. In other words they applied the scientific method. Chance was also a factor, as it is for any new discovery. Are all these researchers thinking that they don’t need to apply the scientific method, or that they can make a new discovery every time they produce a new assay?
This is about antibody results, not virological assays. It’s in these slides: http://www.cfids.org/webinar/slides-121710.pdf
Please give me your defintion of (scientific) evidence. It isn’t hard, but you keep coming up with “answers” that really don’t aswer the question at all.
If you don’t know, just google for it and find a definition you agree with. I think you won’t post any such definition, as it would make your argument vulnerable to criticism, Which, I might add, is a distinctive feature of good science.
Rather, shouting that there is “no evidence” without opening yourself to criticism by not posting your definition of evidence, is much easier.
Please, without further ado, supply us with your definition of evidence (in science).
Again, you completely misrepresent my argument and produce an incoherent reply.
Apologies for the wrong assertion regarding my fake identity, but this is getting silly. Please reread my post. Anyone may disagree, I think the point is pretty clear (and your reply doesn’t address this point at all).
If RRM does not mind me saying so, I think the point is that the original WPI assay was not calibrated against “known positives” either, since no one had done this before. In addition, you now state that the WPI methodology was taken from another source but adapted to blood, with changes to the primers. So somehow in you mind an “adapted” methodology with protocol changes deemed necessary is clearly following the “scientific method”, but another study that in many ways replicates this closely is “unvalidated” if it does not replicate it 100%? Oh yeah.
So based on your own description of the WPI methodology, how and when was it validated? Or does any new methodology automatically get a pass on this issue?
Actually, my post is not self-contradictory. You are fixating on certain details that miss the overall point:
The authors of this study never demonstrated that their assays could detect XMRV in clinical samples (shelf for a moment your concern with “circularity”). You did not show me where they demonstrated this, quite rightly because they did not.
Now we are left, as I pointed out, with *two* variables. Logically and empirically (in this case) there is no way to determine which (or to which extent each) of these variables contributes to the differences in results. Any attempt to assign credit to one over the other is wholly unjustified and purely discriminatory. Yet this is what you and others are doing.
Now let’s return to the “circularity” issue. I first note that the existence of this “circularity” problem has no bearing on my main point (namely, that this study had more than one variable and thus has no real empirical weight). The “circularity” issue is only a problem when trying to eliminate one of the two variables, specifically #2 from my post above. In that regard, the “circularity” issue is purely secondary and your fixation on it serves only to distract from the true issue.
That said, there are ways to square this “circularity.” As I mentioned in another post here, one such way would be to work closely with the WPI to *exactly* duplicate their methods until they could achieve concordant results. Once concordance is achieved, *then* they could systematically and (dare I say) scientifically search for the precise factor causing different results. Maybe it’s a contaminated reagent. Maybe it’s different annealing temperatures. The problem is we still don’t know because these researchers didn’t do anything approaching this level of scientific rigor.
I’m sure there are numerous other ways to get around this “circularity” issue if one is willing to indulge a bit of creativity and ingenuity. Again it boils down to isolating and eliminating unknowns, and the authors here failed to do that on a primary level.
As for your infatuation with a historical example, this issue I’ve outlined is one of very basic logical and scientific reasoning. I’m sure you’re aware that appeals to “the way things have always been done” to justify flawed logic is fallacious. If this were 1978, would you be demanding from me a historical example of when MRI had ever previously been used to diagnose human disease? Paradigms and knowledge change and the past always loses.
“As for your thoughts about my personal motivations concerning all those
things you mention, sorry to sound rude but I frankly couldn’t care
less.”
But that’s just it. Seeing as you’ve posted about 50 responses in this thread, you seem to care very, very much.
Lombardi et al was validated by the four methods used in the study to support the data for Nested RT-PCR. Samples were also tested by the Cleveland clinic and the NCI.
Steve, before you demonize everyone who disagrees with your existing XMRV belief, you should probably realize that at least some of the people you just singled out are actually CFS patients just like you. And next you might note that the only people who appear to be “painstakingly devoted” to any effort are the ones who are voraciously attacking this and any study which appears to question the validity of the WPI results. I personally have no dog in this fight so to speak, it is more of a medical and scientific interest in general.
This isn’t science 101, find out for yourself for a change if you don’t know.
Sorry but you are proposing circular logic.
The authors of the original study did also never demonstrate that they could detect XMRV in clinical samples. It’s the conclusion of their research that they can detect XMRV in clinical samples. This conclusion is either true or false.Once you understand the above, you will understand the circular argument in your post. Please note that your other assertions rely on this circular logic. Also, you sure found a very easy way out of not finding a historical example. But, unlike Gob, who stated that ‘this is the only way in science’, you do at least concede that this very basic logical methodology you propose is unprecented in the history of science as far as you know? Please anwer this very easy question.However, in science, when you propose unprecented methodology, you should produce a paper that explains this new methodology (a blog just won’t do). This paper would have to go through peer review first. Afterwards it would be scrutinized by other scientists and scientific philosophers, and then maybe, maybe, this new, unprecented scientific methodology would be accepted and then you would be regarded as the new Karl Popper of our time. But you are just not there yet….You disregard sound arguments about circular reasoning and propose that the scientific methodology that you’ve made up out of thin air on a forum without critical thinkers is the new way to go in science. It’s not.
Your argument here would only make sense if you claim that XMRV does not exist as an infectious Human retrovirus. Otherwise to prove your methods of detection capable you would have to find it in population level at least. Just like Switzer did and announced this week.
Your belief that XMRV does not exist in one person anywhere in the world is laughable and even the CDC aswell as Isla Singh do not agree with you.
Singh is on video calling it the third human retrovirus and saying it is infectious but the means of infection still need to be worked out.
So again your whole argument of no XMRV or contamination as an explanation for Alter, WPI, CC and NCI labs in ME is laughable. It is laughable because it also relies on your flat earther notion that xmrv does not exist despite the above statements from Isla Sing and the CDC.
You are the one trying to turn this into a circular argument because you are afraid to admit that 0/0 study designers need to go back to the drawing board to prove they are capable of finding the Third Human Retrovirus ( in blood assays) as Dr Singhs herself refers to it, before they commence a study.
– Three labs can routinely and independently find it in a single cohort of banked samples, using (at the time) unvalidated assays.
– No one can find it after that finding.
This really does suggest that something was wrong with those samples:
You are not anwering the question. Please read the question and answer it. It should be very simple if your logic is sound.
You can always provide me with a example of a false finding and I will promise you I can and will explain it using my proposed methodology.
Conclusion: you assert that there is no “evidence “to support a conclusion you don’t like, but are unable or unwilling to state what you think constitutes as “evidence”
I know what is scientific evidence.