In the introduction to their paper, published in the Journal of Virology, the authors note other problems with many of the studies of XMRV in CFS patients:
- Too small control populations
- Patient and control samples collected at different times
- Investigators generally not blinded to sample identity
- PCR assays that rely on conservation of viral sequence mainly used
- Limits of detection, reproducibility, and precision of assays unknown
- Controls for each step that would identify analysis not done
- Insufficient numbers of negative controls included
- No study included positive samples from the original 2009 patient cohort of Lombardi et al.
To address these issues, the authors collected blood from 105 CFS patients and 200 healthy volunteers in the Salt Lake City area. One hundred of the patients fulfilled both the CDC-Fukuda and the Canadian consensus criteria for diagnosis of ME/CFS. The patients were selected from a clinic that specializes in the diagnosis and management of CFS and fibromyalgia.
New blood samples were also collected (by a third party) from 14 patients from the original study by Lombardi et al. The samples were blinded for subsequent study. Detection of viral nucleic acids was done using four different PCR assays. Anti-XMRV antibodies in patient sera were detected by ELISA. Finally, virus growth from clinical specimens was attempted in cell culture. The authors used the multiple experimental approaches reported by Lombardi and colleagues.
Let’s go through the results of each assay separately.
PCR for viral nucleic acids. Four different quantitative PCR assays were developed that detect different regions of the viral genome. The assay for pol sequences has been used by several groups and is the most specific PCR assay for XMRV. Three other PCR assays were also used that target the LTR, gag and env regions of XMRV DNA. These assays could detect at least 5 viral copies of XMRV DNA. The precision and reproducibility of the PCR assays, as well as their specificity for XMRV, were also demonstrated. DNA prepared from white blood cells of 100 CFS patients and 200 controls were negative for XMRV. For every 96 PCR reactions, 12 water controls were included; these were always negative for XMRV DNA.
XMRV antibodies in human sera. To detect XMRV antibodies in human serum, a portion of the viral envelope protein, called SU, was expressed in cells and purified from the cell culture medium. The SU protein was attached to plastic supports, and human serum was added. Any anti-XMRV antibodies in human sera will attach to the SU protein and can subsequently be detected by a colorimetric assay (we have discussed this type of assay previously). This assay revealed no differences in the amount of bound human antibodies for sera from CFS patients or healthy controls. Some of the patient sera were also used in western blot analysis. Recombinant XMRV SU protein was fractionated by gel electrophoresis. The protein on the gel is then transferred to a membrane which is mixed with human serum. If there are anti-XMRV antibodies in the human serum, they will react with the SU protein on the membrane, and can be detected by a colorimetric assay. When rabbit anti-XMRV serum was used in this assay, the SU protein was readily detected. None of the human sera analyzed by this method were found to contain antibodies that detect SU protein.
Infectious XMRV in human plasma. It has been suggested that the most sensitive method for detecting XMRV in patients is to inoculate cultured cells with clinical material and look for evidence of XMRV replication. The XMRV-susceptible cell line LNCaP was therefore infected with 0.1 ml of plasma from 31 patients and 34 healthy volunteers; negative and positive controls were also included. Viral replication was measured by western blot analysis and quantitative PCR. No viral protein or DNA was detected in any culture after incubation for up to 6 weeks.
Analysis of previously XMRV-positive samples. Blood was drawn from twenty-five patients who had tested positive for XMRV as reported by Lombardi et al. These samples were all found to be negative for XMRV DNA and antibodies by the PCR and ELISA assays described above. In addition, no infectious XMRV could be cultured from these 25 samples.
Presence of mouse DNA. After not finding XMRV using qPCR, serological, and viral culture assays, the authors used the nested PCR assay described by Lo et al. Although positives were observed, they were not consistent between different assays. This led the authors to look for contamination in their PCR reagents. After examination of each component, they found that two different versions of Taq polymerase, the enzyme used in PCR assays, contained trace amounts of mouse DNA.
Given the care with which these numerous assays were developed and conducted, it is possible to conclude with great certainty that the patient samples examined in this study do not contain XMRV DNA or antibodies to the virus. It’s not clear why the 14 patients resampled from the original Lombardi et al. study were negative for XMRV in this new study. The authors suggest one possibility: presence of “trace amounts of mouse DNA in the Taq polymerase enzymes used in these previous studies”. I believe that it is important to determine the source of XMRV in samples that have been previously tested positive for viral nucleic acid or antibodies. Without this information, questions about the involvement of XMRV in CFS will continue to linger in the minds of many non-scientists.
At the end of the manuscript the authors state their conclusion from this study:
Given the lack of evidence for XMRV or XMRV-like viruses in our cohort of CFS patients, as well as the lack of these viruses in a set of patients previously tested positive, we feel that that XMRV is not associated with CFS. We are forced to conclude that prescribing antiretroviral agents to CFS patients is insufficiently justified and potentially dangerous.
They also note that there is “still a wealth of prior data to encourage further research into the involvement of other infectious agents in CFS, and these efforts must continue.”
Clifford H. Shin, Lucinda Bateman, Robert Schlaberg, Ashley M. Bunker, Christopher J. Leonard, Ronald W. Hughen, Alan R. Light, Kathleen C. Light, & Ila R. Singh1* (2011). Absence of XMRV and other MLV-related viruses in patients with Chronic Fatigue Syndrome. Journal of Virology : 10.1128/JVI.00693-11

The more serious answer is that the scientific literature shows that many different pathogens can trigger ME/CFS. Improvement with anti-virals doesn’t mean XMRV exists, however.
It does suggest that another virus or combination of pathogens may be involved. Researchers such as Columbia University’s Ian Lipkin and Stanford University’s Jose Montoya are looking at many different viruses in ME/CFS patients.
Self report is not the best way to measure improvement. “I feel better” may reflect the actual patient experience, but good science controls for as many variables as possible.
For example, one way is to measure markers such as immune system abnormalities found in subgroups of ME/CFS patients and see if they change after a well controlled course of anti-virals or immune modulators such as Ampligen. Even better, other researchers have longitudinally followed patients from acute illness phases and then continued to follow the subset of patients that then contracted ME/CFS. A pilot study of anti-virals in such a cohort may well be indicated.
Several pilot studies of anti-virals in subgroups of ME/CFS have been done and have controlled for many of these variables, however a blanket prescription of an anti-viral is questionable at this time and anecdotal evidence, no matter how encouraging, is not the same thing as objective scientific evidence from clinical trials.
It’s a bit of circular logic, isn’t it, to call those patient samples “known positives” when the very issue at hand was whether they were in fact positive in the first place?
The same it has always been for all scientists.
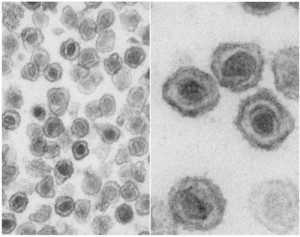
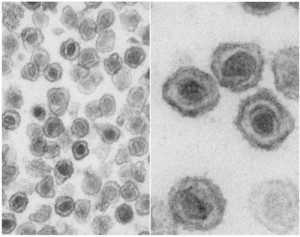
Dr Singhs assays could not detect XMRV in clinical positives from the WPI. She only tested two postive samples from the Lombardi cohort. One of those patients was the source of a sequenced infectious clone and the famous EM image of the budding virus.
She should have said that only two of her patient samples had been shown to be XMRV positives. She used entirely different cycling conditions to Lombardi, Urisman and Lo/Alter.
Even worse she did not use the cycling conditions used by her coleague Schalberg who had detected XMRV in prostate cancer samples. She did not even use the XMRV specific antisera created by Schalberg which was able to detect XMRV in prostate cancer tissue. Schalberg used different forward and reverse primers to account for sequence variability. Singh did not. She claimed that she could not find polytropic sequences when she did not even look for them. This study in fact proves that being able to detect low copy number of VP-62 in a spiked sample does not mean that the assay can detect a polytropic or polytropic/xenotropic MLV in an infected person.
Yes, including the info on their nested PCR: http://www.sciencemag.org/content/suppl/2009/10/08/1179052.DC1/Lombardi.SOM.pdf
The Singh methods are here:
http://jvi.asm.org/cgi/reprint/JVI.00693-11v1.pdf
These scientists do.
“Design and validation of the seminested real-time PCR
methods. Since the sensitivity of single-step real-time (RT-)PCR
methods was suboptimal for the quantitative detection of
HIV-1 RNA and DNA in PBMC from patients undergoing
HAART”
“Detection and quantitation of HIV-1 DNA and RNA in clinical
samples. We proceeded with the validation of the developed
methods to assess their power of detection and quantitation
of HIV-1 RNA and DNA in clinical samples. First, we
validated the usRNA assay by using blood plasma samples
from HIV-infected patients (n 18) with plasma HIV-1 RNA
loads previously measured by a commercial assay (Amplicor).”
They have always shared samples, but those who have received them strangely enough decided not to report the findings.
The February 2011 study by Schwitzer et al used both the original Fukuda and the Canadian definition to define the second cohort rather than relying on convenience samples from old studies using the Empiric definition. But, they didn’t use WPI samples although it is possible they re-tested some of the same patients.
Thank you. Now you can see it is not Nested PCR.
I’d be interested to have an official statement released by Ila Singh on whether or not her latest results published in this paper also invalidate her previous research that lead her to take the folloing patent in which she discloses that she found XMRV in:
“XMRV protein was detected in 23% of prostate cancer cases and in 4% of control tissues.”
“Approximately 25% of breast cancers contained either XMRV proviral DNA sequences or XMRV proteins”
From:
(WO/2010/132886) COMPOSITIONS AND METHODS RELATING TO XMRV-RELATED DISEASES AND CONDITIONS
http://www.wipo.int/pctdb/en/wo.jsp?WO=2010132886&IA=US2010035144&DISPLAY=DESC
Does that mean that her methology was also flawed there and will she pusrsue XMRV-related research or not?
In a few minutes/hours, Gob will explain to you that it is perfectly normal to do this without being able to give you a single example in the history of science.
There are no known positives Gob, and it really isn’t a problem in science. You see, the scientists that first reported the association weren’t able to rely on “known positives” for calibration, which means their findings can (at least, if true) be reproduced without using “known positives”.
Kellylatta: Thank you for giving such a thoughtful, detailed, and respectful reply. It is a welcome contrast to the attitudes of some others, who seem to think that snide, dismissive replies are a good way to address patients’ questions and concerns. I really admire Professor Racaniello for his ability to keep a respectful attitude toward all questioners and give balanced, thoughtful replies. This is a sign of a very good teacher, and a compassionate person.
It’s always worth keeping in mind that this patient population has been subject to incredible amounts of abuse, neglect, and dismissal at the hands of medical personnel and public health agencies. That fact doesn’t mean we should be mindlessly humored, which would be as much an insult to our intelligence as being mindlessly dismissed, but it provides useful context for understanding why so many patients are resentful and suspicious of those who claim to speak with “authority.”
ME/CFS patients have legitimate fears that when leads don’t pan out, research will be abandoned entirely instead of redirected into more promising channels; because that’s exactly what happened in the 1980s. I think that’s a major part of the reason why patients so strongly identify the XMRV theory of causation with the legitimacy of the disease itself. We need to feel secure that research will continue wherever it leads, and that a sense of urgency and levels of funding will become more commensurate with the burden of disease that we suffer.
Please note that the scientists you refer to didn’t use the “known positives” to actually validate the finding that they were infected.
It’s really as simple as this: when you do some gravity experiment, you can assume that the law of gravity is true. When you actually want to test if the law of gravity is true, you cannot rely on it to be true beforehand.
V99, please go away. You are an insufferable troll, and this patient is long past tired of your incessant bullying and spamming antics. I, ME/CFS patient of 10 years, repudiate you. Do tell, before you bugger off, where you get the impressive amount of energy, mental clarity and endurance to carry on like you do with 100s and 1000s of posts on multiple forums? I’d love to know your secret. Which disease did you say you have?
And please take that misanthrope Alan Dove with you.
RRM they used positives to create new assays. This is standard practice.
Ila Singh found that 4% in prostate tissues. She seems to disagree with XMRV being present in blood.
You would insist that no sample is known to be positive until those people you have personally chosen state that it is. This is not how science progresses. In the Blood Working Group there are clinically positive samples.
That’s where I’d like a clarification from her: do her results in cancer tissues still stand, or were these flawed as well by contamination?
With unvalidated assays
The problem is you didn’t say positive samples you said “positive clinical samples”, that’s not standard practice for virus assays.
You completely misrepresent what the Blood Working Group does.
The Blood Working group does not use previously reported positives to calibrate assays to. On the very contrary: labs use “static” assays on samples to see if some or all labs will find consensus on (a) “known positive” sample(s). This is entirely different from the (circular) use of “known positives” you promote.
An ironic aside: if you were actually right, the BWG results thus far prove that WPI’s assays are as unvalidated as any other, as their scores in blinded testing were worse than a (XMRV infected or uninfected) monkey would score.
You completely misrepresent what the Blood Working Group does.
The Blood Working group does not use previously reported positives to calibrate assays to. On the very contrary: labs use “static” assays on samples to see if some or all labs will find consensus on (a) “known positive” sample(s). This is entirely different from the (circular) use of “known positives” you promote.
An ironic aside: if you were actually right, the BWG results thus far prove that WPI’s assays are as unvalidated as any other, as their scores in blinded testing were worse than a (XMRV infected or uninfected) monkey would score.
Yes is it. How else do you intend on validating an assay if it has never been shown capable of detecting the virus.
Yes is it. How else do you intend on validating an assay if it has never been shown capable of detecting the virus.
Dear Guest,
I am about to make a mockery of all my claims about wanting nothing but respectful discourse by admitting that I THINK I LOVE YOU.
Dear Guest,
I am about to make a mockery of all my claims about wanting nothing but respectful discourse by admitting that I THINK I LOVE YOU.
The Blood working group has clinically positive samples. That’s how the CDC detected the virus in II a.
The WPI, Cleveland clinic and NCI assays are validated. As is the Lo/Alter ones.
“There is no doubt whatsoever that Dr. Singh and colleagues are able to detect XMRV DNA in clinical specimens. ”
This seems to be an unsubstantiated assertion. Where in the paper did they demonstrate the ability of their assays to detect XMRV in clinical samples? Perhaps their assays *should* detect it, but this was never demonstrated.
In fact, their inability to find XMRV in suspected positive clinical samples (WPI samples) can be interpreted two ways, as I stated in my previous post. Their efforts add nothing but confusion (or feigned certainty for those desperate for this to go away).
One minor point is that these WPI samples were freshly drawn. As we know from the macaque study, XMRV is found transiently in the blood, so the particular samples taken could have been transiently negative.
But the major point is this: the honest thing to do with these WPI samples after finding them negative with their novel assays would have been to work closely with the WPI to exactly duplicate the WPI’s methodology. Once Singh et al can reproduce the findings of the WPI w.r.t. these samples, then they could systematically explore what causes the differing results between the novel assays in this paper and the methods of the WPI.
Instead, they skirted the issue and the world has learned nothing new except a very detailed assay that cannot find XMRV (be it truly there or not).
This doesn’t address my argument at all. Again…
FYI: the WPI abandoned their “Science” PCR assay in the Blood Working Group and instead went with a newly developed qPCR assay.
They are improving their methodology all the time as you would expect any decent scientist to. The NCI is the same. They use clinically positive samples to do this.
They used Fukuda, not Canadian and I have never heard anything about them retesting anyone previously found positive.
you don’t need a clinical sample, you just need the virus (or the infected cells depending on your assay).
So they are lying in the methods? by saying that used nested PCR?
There is nothing stopping her from producing another paper this time with validated assays.
No where would you get a human retrovirus from?
Try getting that through the regulatory authorities as a liscenced diagnostic test
They are very much mistaken. You are not suggesting that the information in Lombardi et al is a lie?
I generally lik broken records, but your circular reasoning is beyond comprehension.
You suggest that Singh must validate her assay using a “known positive” in order to investigate if the “known positive” is truly positive?
Suppose the WPI findings are false, and I am sure you think they are not given the enormous body of supporting evidence, but suppose, just suppose they are, and there is no XMRV in the blood of patients, how on earth could a scientist show this using your (unprecedented) methodology of using “known positives”?
I’m sorry, but how are they “unvalidated” assays? Because they didn’t come up with the result you want? Why is it that there seems to be one and only one method of finding these positive results? If XMRV is truly prevalent in CFS patients, then why does any small deviation from Lombardi invalidate the results?
I point you to this post, which references a patient with CFS who went on to develop CLL and who has tested positive for XMRV and has been taking 3 antiretrovirals for almost a year. It very clearly shows correlation between starting ARVs, symptomatic improvement, improvement in immune markers common in “CFS”, and improvement in markers for CLL. This is not the only report of such occurrence. If XMRV proper isn’t what is being picked up by the WPI, then surely reports such as this indicate the need for further research into a retroviral cause.
http://treatingxmrv.blogspot.com/2011/04/another-perspective.html
(forgot to paste the URL – and yes i know its n of 1, and yes I know its from a presentation at a conference, but since nobody seems to want to do an actual drug trial now – its the best indication there is).
I think that she believes her PC results still stand.
Perhaps she is personally not as convinced as she was beforehand, but given the fact that she doesn’t extend her conclusions in the paper, I feel she thinks the PC results are true.
It’s not unthinkable really. Suppose HIV was ubiquitous in certain lab cell lines and reagents. Surely some scientists would then report false disease associations with HIV. HIV would then still cause AIDS however.
For the record, I personally believe the XMRV-PC connection will not hold up either.
Yet their “improved assays” performed no better than chance would predict in the blinded setting of Phase IIb? Then please give me back the assays that reliably differentiated between CFS patients and healthy controls in the Science paper.
You seem to be very selective in your criticism.
The problem is that you are referring to “it” as if it is evident what “it” is.
Fact is that Lombardi et al. and this Singh study both performed nested PCR assays.
The relevent section from the Singh M&M’s reads: “For the nested PCR, we made 2 modifications to the original protocol (11). We used 1.0 U of 205 Platinum Taq instead of 0.5 U, and added dUTP to the mastermix to prevent subsequent PCR 206 contamination with amplicons”
From Lombardi et al’ supporting online material: “To avoid potential problems with laboratory DNA contamination, nested PCR was performed with separate reagents in a separate laboratory room designated to be free of high copy amplicon or plasmid DNA…PCR amplification for sequencing full-length XMRV genomes was performed on DNA amplified by nested or semi-nested PCR from overlapping regions from PBMC DNA….Nested RT-PCR for gag sequences was done as described (5) with modifications.”
Also, from the very Lombardi et al. paper:
“Using the Whittemore Peterson Institute’s (WPI) national tissue repository, which contains samples from well-characterized cohorts of CFS, we isolated nucleic acids from PBMCs and assayed the samples for XMRV gag sequences by
NESTED
PCR (5, 6). Of the 101 CFS samples analyzed, 68 (67%) contained XMRV gag sequence.”
Keep in mind that correlation does not prove causation.
Not proven capable of detecting a known positive.
The virus is in low levels in the blood as this is not it’s main reservoir. Hence the need to use a method that has sensitivity, not specificity as the other assays targeted at a clone have.
Warmer. It is not hidden information. Other studies have stated what was used.
Again, you completely represent data.
– The CDC did only test for serology according to those slides. Why quote from a wacko conspiracy blog instead from the actual slides?
– Please read the Van Kuppenveld letter again. Van Kuppenveld sent the WPI 10 samples, all of which were negative according to Van Kuppenveld. The WPI tested these samples and found some of them to be positive (like in the BWG, the WPI wasn’t able to differentiate between patients and controls better than a monkey would do, BTW). And THEN, Van Kuppenveld retested his own samples (which WPI thought were positive) and consistently found them to be negative. That is what that letter states. I am not English or American and I can perfectly understand that.
In your circular logic, you could say that WPI didn’t use validated assays on the “known negative samples” of Van Kuppenveld and should have calibrated their assays accordingly (chuckle)….
represent = misrepresent
Doctors were prescribing ARVs years before they isolated HIV. These viruses only have to be present to cause disease.