Chronic fatigue syndrome (CFS) is a disease characterized by fatigue and chronic inflammation that can last years and may affect ~1% of the world’s population. The etiology of the disease is unknown, although several viruses have been suggested to be involved, including enteroviruses and herpesviruses.
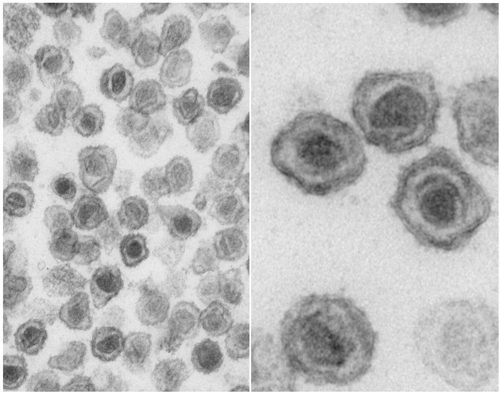
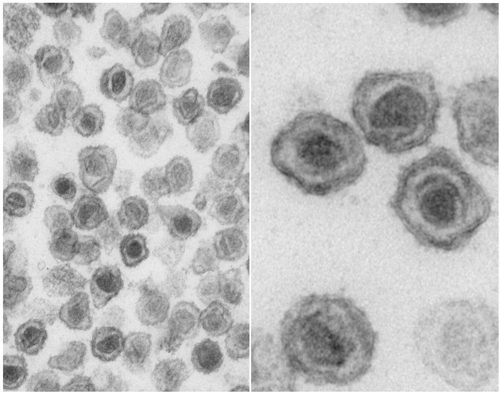
The retrovirus XMRV (xenotropic Moloney murine leukemia virus-related virus) was recently identified in the tumor tissue of individuals with prostate cancer. XMRV nucleic acid was detected by polymerase chain reaction in the blood of 68 out of 101 samples (67%) from CFS patients. The virus was also found in 8 of 213 samples (3.7%) from healthy individuals. Antibodies to the virus were found in 19 of 30 CFS blood samples, but not in 16 healthy control specimens. Viral proteins were identified in both B and T lymphocytes, and infectious virus could be cultured from these cells.
Nucleotide sequence analysis of two XMRV genomes cloned from patient samples revealed that the virus is >99% identical to the virus identified in prostate cancers. Nevertheless, the two XMRV genomes are sufficiently different to suggest that the two CFS patients were independently infected.
These findings must be verified by more extensive analysis of CFS and healthy populations worldwide. But XMRV is real and its presence in people raises many questions.
Where did XMRV come from? The retroviruses identified in patients with CFS or prostate cancer are highly related (more than 90% DNA sequence identity) to a group of viruses of wild and laboratory mice called xenotropic murine leukemia virus. Xenotropic MLVs are endogenous retroviruses of mice – the viral DNA is integrated into the mouse genome. Mice produce low levels of the virus – a few infectious viruses per milliliter of blood – but the virus cannot reinfect mouse tissues (hence the name ‘xenotropic’, meaning a virus that can grow in species other than that of its origin). These viruses can infect many cells, including human cells. Therefore it is not unreasonable to hypothesize that XMRV is a xenotropic MLV that crossed from mice to humans. Remember the zoonotic pool?
Does XMRV cause CFS? While the presence of XMRV in 67% of CFS samples seems impressive, it could be misleading. For example, the samples could be from regions where XMRV infection is common. Alternatively, patients with CFS could be more susceptible to infection. This is why more extensive epidemiological studies must be done.
How would XMRV be transmitted? Since XMRV is in the blood, it could be transmitted via transfusion, intravenous drug use, or by any other blood-borne route. Whether or not other modes of transmission (respiratory, sexual) are involved depends on where else the virus is found in humans.
How would XMRV cause disease? One idea is that infection with XMRV, which is present in high titers in the blood, leads to a continuous, long-term immune response. Think about how you feel during the 5 days of an influenza virus infection. A vigorous immune response exhausts the body, especially when it is chronic.
Many CFS patients develop cancer. It will be interesting to determine if XMRV integration into human DNA activates oncogenes, leading to cell transformation.
What about the 3.7% of healthy people who have XMRV? If this number is representative of the general population, then many millions of individuals would harbor the virus. XMRV could be involved in other diseases of unknown origin.
It will take time to answer the many questions raised by the discovery of XMRV. The good news is that some of the anti-retroviral drugs licensed for treating AIDS can be immediately tested for their efficacy against CFS.
Urisman A, Molinaro RJ, Fischer N, Plummer SJ, Casey G, Klein EA, Malathi K, Magi-Galluzzi C, Tubbs RR, Ganem D, Silverman RH, & DeRisi JL (2006). Identification of a novel Gammaretrovirus in prostate tumors of patients homozygous for R462Q RNASEL variant. PLoS pathogens, 2 (3) PMID: 16609730
Lombardi VC, Ruscetti FW, Das Gupta J, Pfost MA, Hagen KS, Peterson DL, Ruscetti SK, Bagni RK, Petrow-Sadowski C, Gold B, Dean M, Silverman RH, & Mikovits JA (2009). Detection of an Infectious Retrovirus, XMRV, in Blood Cells of Patients with Chronic Fatigue Syndrome. Science (New York, N.Y.) PMID: 19815723
Schlaberg R, Choe DJ, Brown KR, Thaker HM, & Singh IR (2009). XMRV is present in malignant prostatic epithelium and is associated with prostate cancer, especially high-grade tumors. Proceedings of the National Academy of Sciences of the United States of America, 106 (38), 16351-6 PMID: 19805305

Also of interest to researchers is that retroviruses are known to reactive latent viruses.
For nearly 30 years, biomedical research has pointed to HHV-4 and HHV-6A as having high viral loads as well as reactivation in CFS patients (as defined using the 1988 Holmes definition, then the 1994 Fukada definition or finally the 2003 Canadian Consensus which is known to select a far sicker subset.)
The latter two were the definitions used to select CFS patients for the Lombardi et al XMRV study in patients with CFS. Twenty years ago microbiologists were looking at what they thought was a new retrovirus in CFS patients. Technology has made tremendous leaps since then. Just think. What if?
Vince also mentions geography. More extensive studies in other geographical areas goes without saying. For example Burkitt's lymphoma which is caused by EBV is found primarily in Africa I believe, but scientists also know that the presence of HHV-6A in that cancer is the biological equivalent of throwing gasoline on a bonfire. So can reactivated latent viruses determine who is sicker or what form their disease takes?
However the reason these two disparate groups in Lombardi et al were looked at is because both patients with XMRV prostrate cancer and CFS patients were found to have a similar although not exact defect in RNaseL pathways. Once again, going back years, this RNaseL pathway has been documented in the sickest subsets of CFS patients all over the world. Yet another clue in a tantalizing puzzle.
Other viruses found in these subsets of patients in recent years include parvovirus as well as others including polio virus in a few studies. This has implications regarding whether XMRV is a passenger or the smoking gun in this particular neuroimmune disease as well as other chronic diseases.
Or take genetics, Kerr et al, defining the CFS patient group the same way as Lombardi et al, found that highly represented functions were hematological disease and function, immunological disease and function, cancer, cell death, immune response and infection. More clues? The hunt is on.
What fun to be able to watch history unfold.
You have mentioned very important and useful points in your article and i am glad to be part o fit.'
Tia Smith
wow gold
Is XMRV lipid enveloped? If so, is it possible to dissolve it using monolaurin (lauric acid)?
Yes, XMRV has a lipid envelope. Lauric acid is a fatty acid, some of which are known to have virucidal activity. Whether or not it disrupts XMRV would have to be determined; it does not disrupt another enveloped virus, arenavirus, for example.
thank you for the article. what aids drugs do you think might be tested for use in CFS and when would they be available for use in CFS?
I don't know what Vince would say, but according to the testimony Dr. John Coffin, a retrovirus expert with the NCI and Tufts University, gave yesterday the odds are higher for a vaccine in the case of XMRV. According to Dr. Coffin, one of the interesting things about XMRV is just how close the XMRV virus is in patients with prostate cancer and chronic fatigue syndrome. This means there are fewer cycles of replication. In respect to your specific question Dr. Coffin stated that this means that XMRV patients may not respond to HIV anti-virals, but it makes it easier to develop a vaccine. However immune modulators developed for patients with HIV may be effective.
The nucleoside analogs such as AZT, ZDV, ddI and the like are most likely to inhibit XMRV replication. Non-nucleoside inhibitors, fusion, and protease inhibitors probably won't work as they are specific for HIV-1. As these are all approved for use against HIV they could in theory be prescribed 'off label' today to treat XMRV infection.
If you're already infected with XMRV it's not clear that a vaccine would be useful; in those cases antivirals would probably be preferred. A vaccine would be great to prevent infection – but who would get it? Depends upon who is at risk for XMRV infection.
– Would you be able to comment on the circulating rumor that the 67% prevalence reported in Science has been revised to something closer to 95%?
– Also, do you have any thoughts on the seemingly more general phenomenon of “post viral-illness fatigue”? This is something discussed in connection with several viral illnesses including AIDS and Q-fever.
Thanks very much!
Rumor no more. Dr. Dan Peterson testified regarding the 33 patients who did not initially show XMRV at a Washington DC NIH/DHHS hearing on October 29, 2009. There is also interesting testimony by Dr. John Coffin who has been studying retroviruses for 45 years. http://videocast.nih.gov/PastEvents.asp
Recap provided by Dr. David Bell whose patients were among those examined by the WPI team and who first indentified 60 children who contracted ME/CFS in a cluster outbreak in Western New York in 1985.
“XMRV DNA was found from 68 of 101 patients (67%), and this was in the Science paper. That leaves 33 patients with CFS who were negative. But on further testing 19 of these 33 are XMRV antibody positive, 30 of these 33 had transmissible virus in the plasma, and 10 of these 33 had protein expression. Overall 99 of the 101 patients show evidence of XMRV infection.
These results have interesting implications. The most important is that there is not a simple test now that will tell you if you have XMRV or if the virus is active in your system. And we need a good control study using all three measures to accurately know control presence of the virus. Right now, it is necessary to do several tests to know the XMRV status:
a) DNA by PCR
b) Viral infectivity
c) Detection of viral proteins
d) Antibody to the XMRV envelope…”
http://www.davidsbell.com/
Also in testimony: the NCI, in as yet unpublished findings, has replicated the XMRV findings in patients with ME/CFS. In a cohort entirely unrelated to the WPI cohort they found 9 of 15 ME/CFS patients positive by PCR and 13 of 15 were positive by culture technique.
XMRV was also found using at least one of the three techniques as follows:
Atypical MS: 3 out of 3 were positive.
Fibromyalgia: 12 out of 20 were positive.
Autism: 6 out of 15
GWI: not tested
I wonder if anyone might like to comment on the nature of the perceived fatigue in CFS. Fatigue is something very familiar, of course, but, perhaps in this day and age, a bit intellectually stunted as either a medical or physiological concept. It is a very commonly reported symptom, but one with almost no real diagnostic value. It seems that persistent fatigue is being noted following several other viral illnesses besides chronic fatigue syndrome, including HIV. I don't know precisely how one distinguishes between fatigue and brain fog for that matter. But, these are both debilitating conditions that affect a huge number of people. Maybe there is an opportunity to get at the mind-brain connection?
You are of course correct that the word choice of undefined fatigue is vague and should probably be abandoned. I believe fatigability and exhaustion are the actual medical terms. However, fatigue, is a commonly reported symptom of viral illness regardless of how it is defined.
What makes it unique in the case of patients with CFS, is that it is post-exertional fatigue unrelieved by rest and lasting at least 24-hours. Post-exertional malaise and/or fatigue of inappropriate severity can temporarily immobilize the patient and worsen her/his symptoms following normal physical or mental activity. It takes the patient an inordinate amount of time to recover – 24 hours or more. De Becker et al assessed 2073 consecutive patients with major complaints of prolonged fatigue. Of the 1578 patients that met the (1994) Fukuda criteria, 97.3% had post-exertional malaise with a severity of 2.7 out of three. Of the 951 who met the Holmes criteria, 98.8% had post-exertional malaise with a severity of 2.8 out of 3. (It should be noted that the original 1988 Holmes definition contained many symptoms and signs common to viral illness.)
It could be argued that changing the definition doesn't change the disease, it simply confounds research results.
As De Becker et al, and many others, have shown, how fatigue is defined (severity and duration are always key in a differential diagnosis) makes a substantial difference in not only diagnostic value, but in what patients are actually being studied.
And, as Dr. Nancy Klimas stated in a March 24, 2009 interview with the Miami Herald regarding symptoms of CFS, “The big one would be post-exertional relapse. There aren’t many illnesses that get worse when you exercise…”
A postexertional relapse connection to the mind? Sorry, I couldn't find any research to support that hypothesis. Perhaps someone else knows of some.
Brain fog is also colloquialism that can also mean many things to many people. In CFS patients, perhaps not surprisingly, cognitive processing becomes more impaired in response to challenging physical exertion according to LaManca et al. The most common cognitive problems in CFS have been shown to be slowed processing speed, deficits in working memory and in some patients very high alpha amplitudes in their occipital and temporal regions per Harvard neurologist Frank H. Duffy in unpublished data. Duffy notes that these clinical findings are also consistent with head injury, extreme sleep deprivation, and encephalopathy. The findings were distinct from sleepy or depressed controls.
The question then might be what viruses or combination of activated viruses in CFS patients are neurotropic and what might their role be?
De Becker P, McGregor N, De Meirleir K. A definition-based analysis of symptoms in a large cohort of patients with chronic fatigue syndrome. J Intern Med 2001;250:234-240
La Manca JJ, Sisto SA, DeLuca J, Johnson SK, Lange G, Pareja J, Cook S, Natelson BH. Influence of exhaustive treadmill exercise on cognitive functioning in chronic fatigue syndrome. Am J Med 1998 Sept 28;105(3A):59S-65S.
Lange G, Steffener J, Cook DB, Bly BM, Christodoulou C, Liu WC, Deluca J, Natelson BH. Objective evidence of cognitive complaints in Chronic Fatigue Syndrome: a BOLD fMRI study of verbal working memory. Neuroimage. 2005 Jun;26(2):513-24. Epub 2005 Apr 7.
You are of course correct that the word choice of undefined fatigue is vague and should probably be abandoned. I believe fatigability and exhaustion are the actual medical terms. However, fatigue, is a commonly reported symptom of viral illness regardless of how it is defined.
What makes it unique in the case of patients with CFS, is that it is post-exertional fatigue unrelieved by rest and lasting at least 24-hours. Post-exertional malaise and/or fatigue of inappropriate severity can temporarily immobilize the patient and worsen her/his symptoms following normal physical or mental activity. It takes the patient an inordinate amount of time to recover – 24 hours or more. De Becker et al assessed 2073 consecutive patients with major complaints of prolonged fatigue. Of the 1578 patients that met the (1994) Fukuda criteria, 97.3% had post-exertional malaise with a severity of 2.7 out of three. Of the 951 who met the Holmes criteria, 98.8% had post-exertional malaise with a severity of 2.8 out of 3. (It should be noted that the original 1988 Holmes definition contained many symptoms and signs common to viral illness.)
It could be argued that changing the definition doesn't change the disease, it simply confounds research results.
As De Becker et al, and many others, have shown, how fatigue is defined (severity and duration are always key in a differential diagnosis) makes a substantial difference in not only diagnostic value, but in what patients are actually being studied.
And, as Dr. Nancy Klimas stated in a March 24, 2009 interview with the Miami Herald regarding symptoms of CFS, “The big one would be post-exertional relapse. There aren’t many illnesses that get worse when you exercise…”
A postexertional relapse connection to the mind? Sorry, I couldn't find any research to support that hypothesis. Perhaps someone else knows of some.
Brain fog is also colloquialism that can also mean many things to many people. In CFS patients, perhaps not surprisingly, cognitive processing becomes more impaired in response to challenging physical exertion according to LaManca et al. The most common cognitive problems in CFS have been shown to be slowed processing speed, deficits in working memory and in some patients very high alpha amplitudes in their occipital and temporal regions per Harvard neurologist Frank H. Duffy in unpublished data. Duffy notes that these clinical findings are also consistent with head injury, extreme sleep deprivation, and encephalopathy. The findings were distinct from sleepy or depressed controls.
The question then might be what viruses or combination of activated viruses in CFS patients are neurotropic and what might their role be?
De Becker P, McGregor N, De Meirleir K. A definition-based analysis of symptoms in a large cohort of patients with chronic fatigue syndrome. J Intern Med 2001;250:234-240
La Manca JJ, Sisto SA, DeLuca J, Johnson SK, Lange G, Pareja J, Cook S, Natelson BH. Influence of exhaustive treadmill exercise on cognitive functioning in chronic fatigue syndrome. Am J Med 1998 Sept 28;105(3A):59S-65S.
Lange G, Steffener J, Cook DB, Bly BM, Christodoulou C, Liu WC, Deluca J, Natelson BH. Objective evidence of cognitive complaints in Chronic Fatigue Syndrome: a BOLD fMRI study of verbal working memory. Neuroimage. 2005 Jun;26(2):513-24. Epub 2005 Apr 7.
Now that a clinical laboratory assay for XMRV is being made available, and that DHHS, CDC, SSA, NCI, and many other federal agencies, are paying attention to these scientific developments, what recommendations are our public health authorities, and other trusted national infectious diseases experts, making to the public?
Here is a magnificent opportunity for data to be rapidly collected and analyzed. DHHS might even consider directly paying for these tests as part of a large clinical evaluation and save everyone from having to appeal this to their manifold insurance carriers one by one.
I pray this will lead to healing for all of us sufferers of CFS. I have been ill since I was 15, and I'm now 43! The last 15 years have been the worst. I've also had breast cancer. But good news and breakthrough are on the way!
Pingback: Raltegravir inhibits murine leukemia virus: implications for chronic fatigue syndrome?
I am so happy to read all of this information. Brenda, like you I've had CFS since my late 20's. I've had every test imaginable. Breast cancer twice, and now at 56 am so thankful this virus has been identified. Now, at least, I can make some sense of the last almost 30 years.
Could anyone address the question about heredity? Is it possible that I may have passed this along to my children? They were born about ten years after my symptoms began occurring.
Thank you all for your very valuable information.
No, famciclovir is not active against retroviruses such as XMRV and
hence cannot be used to treat CFS.
That's a very interesting question – whether XMRV has entered the
human germline. There is no evidence so far that it has and therefore
I would say that the infection cannot be passed vertically, that is
from parent to offspring. In mice, MLV, which is most likely the
progenitor of XMRV, is part of the germline and is passed by heredity.
I am sure we will know very soon whether XMRV has integrated into
human germline cells.
Any anonymous comments or speculations from clinicians regarding possible antiviral treatments based on our 30 year experieve with HIV? Certainly, if one believes that XMRV is behind chronic fatigue syndrome, ampligen is held by many CFS-clinicians as having been effective for CFS pts. Others also believe valcyte to be effective. I really cannot believe that the FDA won't approve ampligen after having come this far. Asking for more toxicity data strikes me a final precautionary step before approval. Lack of efficacy surely would have stopped the process by this point. Come on clinicians, these pts need to be treated. There is an adverse impact involved in doing nothing.
But it could still be passed vertically in utero, like HIV, right? Without infecting the germ line?
Thankyou for the information Profvrr. Perhaps I should ask if there are any
available (not necessarily particular to though) anti-viral (or otherwise)
treatment/medication that are active against XMRV?
Also, do you know of any prescription medication for the latent form of the
EBV (Epstein Barr Virus), which as I understand is present in a significant
portion of the population, and may also be realated to CFS in some
individuals.
Thank You,
Adam.
Yes, in theory, XMRV could be passed vertically – to do so it would
have to cross the placenta.
I understand that AZT and raltegravir are active against XMRV. None of
this is yet published and I expect in the coming months to see more in
the literature on this question. As for latent EBV, Valacyclovir is
the antiviral of choice to treat active infection. In a recent paper
in the Journal of Virology, it was shown that Valacyclovir reduces the
frequency of EBV-infected B cells when administered over a long
period. In theory this might allow eradication of EBV from the body if
reinfection does not occur.
Actually, one study that was just published exploring the efficacy of AZT as it relates to XMRV shows up in PubMed.
Virology 2009 Dec 1.
http://www.ncbi.nlm.nih.gov/sites/entrez
Xenotropic murine leukemia
virus-related virus is susceptible
to AZT.
Sakuma R, Sakuma T, Ohmine S, Silverman
RH, Ikeda Y.
Department of Molecular Medicine, Mayo Clinic, 200
First Street SW, Rochester, MN 55906, USA.
The xenotropic murine leukemia virus-related virus
(XMRV) is a human retrovirus, recently isolated from
tissues of prostate cancer patients with impaired
RNase L activity.
In this study, we evaluated 10 licensed anti-HIV-1
compounds for their activity against XMRV, including
protease inhibitors (PI), nucleoside reverse
transcriptase (RT) inhibitors (NRTI), non-nucleoside
RT inhibitors (NNRTI) and an integrase inhibitor.
No PI affected XMRV production; even high
concentrations of Ritonavir failed to inhibit the
maturation of XMRV Gag polyproteins.
Among the NRTI, NNRTI and integrase inhibitors
used in this study, only AZT blocked XMRV infection
and replication through inhibition of viral reverse
transcription.
This sensitivity of XMRV to AZT may be explained by
the modest homology in the motif D sequences of
HIV-1 and XMRV reverse transcriptases.
If XMRV becomes established as an etiological agent
for prostate cancer or other diseases, AZT may be
useful for preventing or treating XMRV infections in
humans.
PMID: 19959199 [PubMed – as supplied by publisher]
As a scientist on another list has noted about AZT:
“…For information, the following is a quotation of the FDA-required black box
warning in the 2008 edition of the Physician's Desk Reference, page 1560,
under Retrovir (zidovudine) [also known as AZT]:
“WARNING
RETROVIR (ZIDOVUDINE) HAS BEEN ASSOCIATED WITH HEMATOLOGIC TOXICITY
INCLUDING NEUTROPENIA AND SEVERE ANEMIA PARTICULARLY IN PATIENTS WITH
ADVANCED HUMAN IMMUNODEFICIENCY VIRUS (HIV) DISEASE.
PROLONGED USE OF RETROVIR HAS BEEN ASSOCIATED WITH SYMPTOMATIC MYOPATHY.
LACTIC ACIDOSIS AND SEVERE HEPATOMEGALY WITH STEATOSIS, INCLUDING FATAL
CASES, HAVE BEEN REPORTED WITH THE USE OF NUCLEOSIDE ANALOGUES ALONE OR IN
COMBINATION, INCLUDING RETROVIR AND OTHER ANTIRETROVIRALS.”
As in if it don't kill ya it may cure ya.
Thanks for that. Interesting. Note they are looking at XMRV from the
point of view of prostate cancer; when they submitted the paper in
September the CFS report had not yet come out in Science. Otherwise
they would have mentioned CFS in the paper.
i just found this info on xmrv and cfs. what tests would one ask for as my doctor knows nothing about this and what is the treatment. thanks
Tom,
Information regarding commercially available XMRV tests your doctor could order are not widely available as there is no standard at this time. However the Whittemore-Peterson Institute is temporarily allowing Viral Immune Pathology Diagnostics (VIP Dx) in Reno NV to offer the same test they used for their breakthrough study. More information is available at http://www.vipdx.com
Please keep in mind however, that no matter how much potential the XMRV study regarding patients with the neuroimmune disease CFS may have, there is currently no specific evidence that XMRV causes any disease in humans. Association is not causation.
Excellent stuff, thank you. The information is very much appreciated.
Is is possible that XMRV virus crossed from wild mice to domesticated cats to pet cat owners via scratches or bites from pet cats? Is there any known correlation of CFS patients as having a higher than normal incidence as cat owners? Has anyone ever tested a pet cat for XRMV virus? Thank you.
There is some research being done on a link between another murine virus and human breast cancer.
http://www3.interscience.wiley.com/journal/1121…
Of mice, cats, and men: Is human breast cancer a Zoonosis?
Keywords
mouse mammary tumor virus (MMTV) • betaretroviridae • feline • breast cancer
XMRV- also mentions it's a form of Lukemia in mice. My question is the fact that CFS paitients have gotten cancer, could there be some sort of connection between Lukemia and this XMRV?
I have Fibromyalgia and was dx 1 year ago. My daughter tested paoitive for Epstein Barr. My mother has Lukemia, as did my grandmother and my great great grandmother. Is there some sort of DNA hereditary issue here?
A very good friend with ME/CFS was diagnosed with breast cancer. I'm not quite sure how to ask this question but I see that you have walked this road. How did your body handle radiation/chemo/surgery when you are already depleted? Do you have resources, help, hope I can give her?
What about passing on the virus within breast milk? Could this not also be a common way to pass on the virus, especially considering the fact that XMRV is now thought to be present within distinct populations (mainly because CFS occurs within high density in some areas and not in others)?
Pingback: XMRV linked to CFS/ME and Fibromyalgia? « Vanish Despair
All of this is very interesting since I have been plagued with a host of immune diseases starting with chronic fatigue, cancer, fibromyalgia, Epstein Barr, leading on into AIDS. I search for some common thread in all of this. Have struck out with HHV6, which I don't have either variant of the virus, but then what causes my immune issues? I have found though, that the anti-virals or HAART does suppress the fatigue and fibromyalgia symptoms. Hopefully, further research will shed more light on the issue and bring resolution to those who suffer.
All of this is very interesting since I have been plagued with a host of immune diseases starting with chronic fatigue, cancer, fibromyalgia, Epstein Barr, leading on into AIDS. I search for some common thread in all of this. Have struck out with HHV6, which I don't have either variant of the virus, but then what causes my immune issues? I have found though, that the anti-virals or HAART does suppress the fatigue and fibromyalgia symptoms. Hopefully, further research will shed more light on the issue and bring resolution to those who suffer.
Pingback: XMRV, prostate cancer, and chronic fatigue syndrome
The following statement in your blog post is being cited on a patient forum to justify patients who are taking AZT and other anti-retrovirals for CFS right now, outside of any clinical trial or research setting. At least one of these patients taking anti-retrovirals even tested negative for XMRV. I hope you will clarify your thoughts on this matter and whether your statements should be interpreted as endorsements of untested medical treatments for an illness whose association with the retrovirus XMRV has not yet been confirmed much less proven to be causal.
“It will take time to answer the many questions raised by the discovery of XMRV. The good news is that some of the anti-retroviral drugs licensed for treating AIDS can be immediately tested for their efficacy against CFS.”
http://www.forums.aboutmecfs.org/showthread.php…
http://www.forums.aboutmecfs.org/showthread.php…
Pingback: a follow-up on bleeding for the cause | BioBlog
You could point out to them that the original post said:
“Does XMRV cause CFS? While the presence of XMRV in 67% of CFS samples seems impressive, it could be misleading. For example, the samples could be from regions where XMRV infection is common. Alternatively, patients with CFS could be more susceptible to infection. This is why more extensive epidemiological studies must be done.”
Neither the WPI study nor any other scientific or medical orgaization is suggesting that we can know XMRV causes CFS. We can't know that, and it may well not. We don't even know for sure if XMRV causes any symptoms. All we know is that we sometimes find it significantly more often in certain patient populations and sometimes don't find it associated with any disease. Nobody should be using anti-retroviral drugs for CFS unless it can be shown through proper, controlled clinical trials to be helpful. But right now we don't even know enough to run clinical trials. Anti-retroviral drugs aren't safe to experiment with. You can try Omega-3 or tricyclic antidepressants (they can help with pain and sleep even if comorbid depression isn't an issue) or things of that sort without clinical trials, but this isn't a good idea with anti-retrovirals. What doctor do they have rx-ing this?
As a PWC, I understand the urgency of needing an effective treatment, but we have to be patient a little while longer. Treatment for our disease will come. I actually think the cardiovascular theories will provide a useful treatment soonest. Several other theories will hopefully add treatments in time.
Thanks for that very briefly explained post. Very clear and concise. That was very helpful. Keep posting more informative articles like the same.
Just goes to show that everything is holistic and affects everything else. Who would thing that prostate cancer and chronic fatigue have something in common?
wanted to thank you for this great read!! I definitely enjoying every little bit of it I have you bookmarked to check out new stuff you post.
Pingback: Ila Singh finds no XMRV in patients with chronic fatigue syndrome
Pingback: Chronic Fatigue Syndrome in “not caused by single virus” shock! | Brain and Head Health
Ritalin is a prescription drug that is recommended for the treatment of Attention Deficit Disorder or ADHD. It is composed of Methylphenidate which is a narcotic drug and stimulant. This substance stimulates the central nervous system and thereby improves the condition of the patient taking it. Along with treating Attention Deficit Hyperactivity Disorder, it also takes care of other related disorders like chronic fatigue syndrome and narcolepsy. However, owing to its tendency of abuse, Ritalin has been in the middle of many controversies. Since it is the brand name of methylphenidate, it is considered to be illegal to purchase or sell this drug without a prescription.
Look into the research of Dr. Tom Glass, a veterinary pathologist. There is indeed a much greater incidence of contact between ME patients and animals and he did find pathology in the animals (who had symptoms similar to ME) indicative of some sort of infection.
Pingback: Science retracts paper on detection of XMRV in CFS patients
Pingback: Authors retract paper on detection of murine leukemia virus-releated sequences in CFS patients